Sepsis analysis today
Sampling
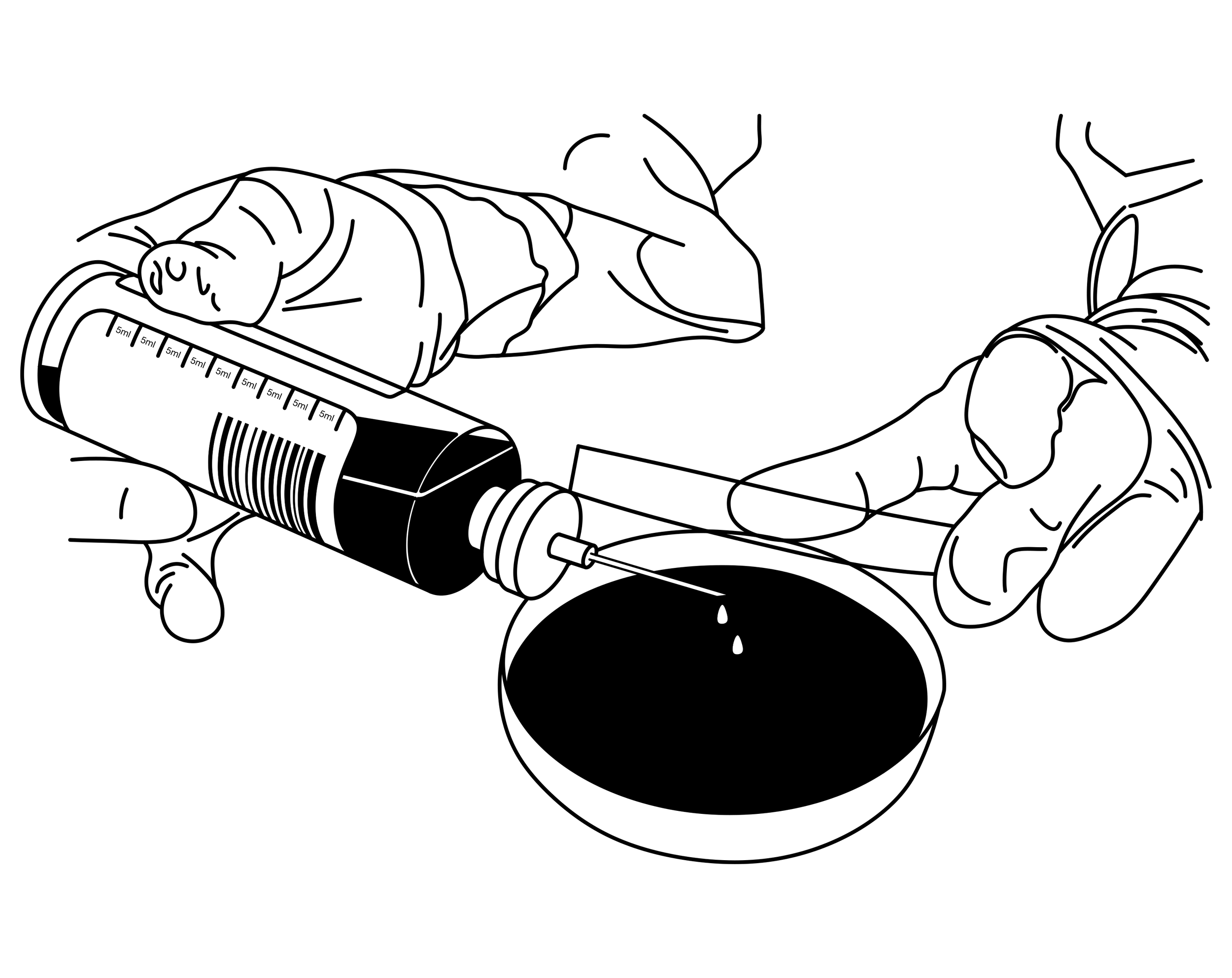
A blood sample for sepsis diagnosis is taken by gathering the necessary materials such as sterile blood culture (BC) bottles, a BC bottle adapter, needles, syringes, alcohol swabs, bandages, and gloves. The injection site is cleaned with an alcohol swab and the procedure is performed while wearing gloves. The blood is drawn through negative pressure in the BC bottle once attached to the patient through the bottle adapter. The gold standard foresees the collection of four bottles each filled with 8-10ml of blood. After the transfer, the BC bottles should be shaken gently to ensure proper mixing of their contents - blood and broth. After labeling the patient's information and the date and time of the sample, it is sent for further analysis to the laboratory as soon as possible. The needle and syringe are disposed of and a bandage is applied to the patient.
Incubation
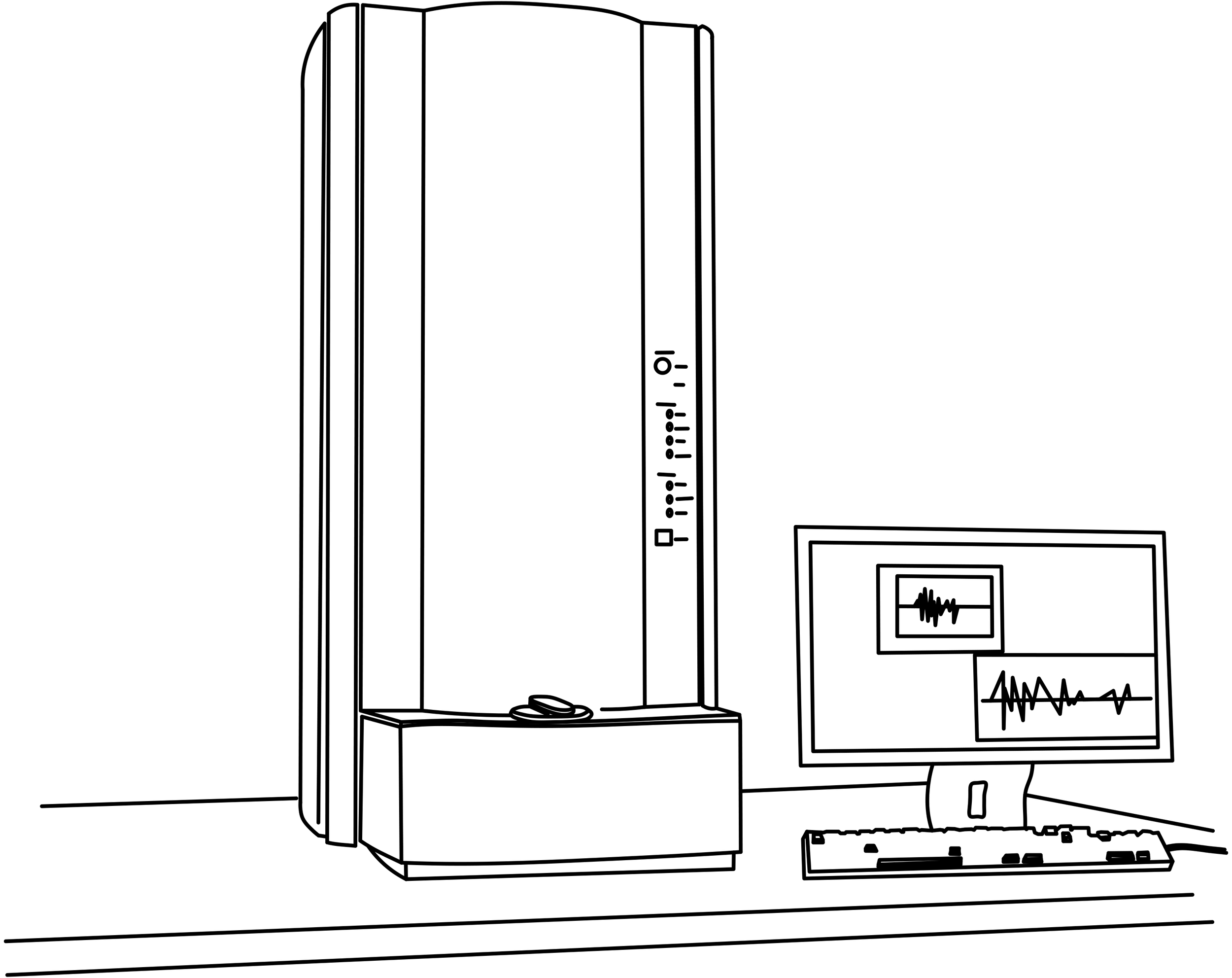
At the laboratory, the BC bottles are incubated in a warm environment at 35-37°C for at least 48-72 hours, or until the broth in the bottle appears turbid - indicating bacterial growth. The bottles are then checked periodically, either manually or using an automated system. In manual systems, this involves visually inspecting the bottles for turbidity or gas production. In automated systems, the growth of bacteria is monitored continuously and the system alerts the laboratory when growth is detected. If bacterial growth is observed, a colony from the bottle is aseptically obtained using a sterile loop or needle and transferred to a new culture medium for identification and antibiotic susceptibility testing. The selected colony should represent the predominant organism in the bottle. It is important to follow proper aseptic techniques when transferring the colony to prevent contamination of the culture.
Interpretation
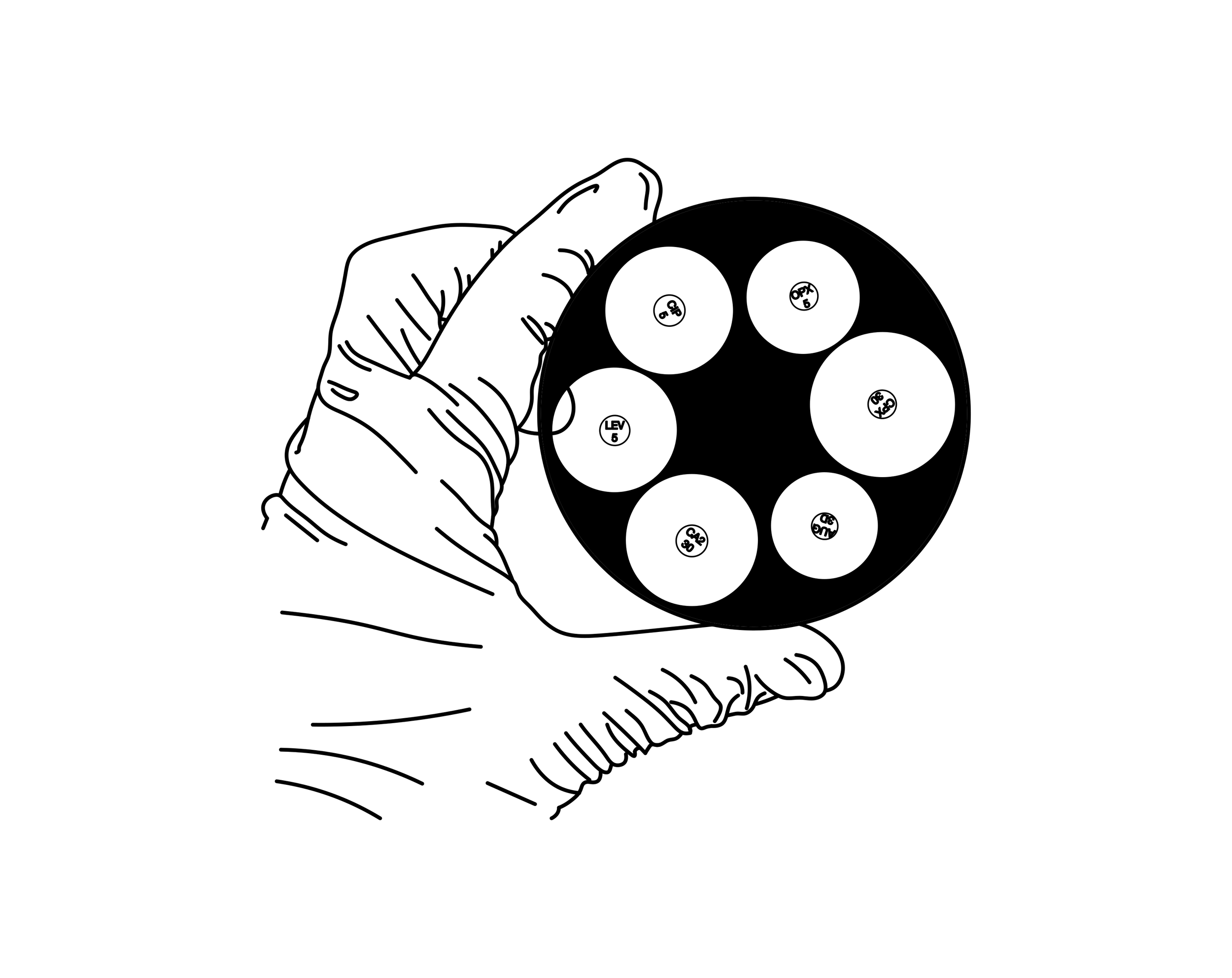
Results from the identification and antibiotic susceptibility testing can then be interpreted to diagnose sepsis, including determining the causative organism and its antibiotic susceptibility pattern. This information can be used to guide the selection of appropriate antibiotics for treatment. The identification of the causative organism can be done using various techniques such as gram staining, biochemical tests, and molecular methods. Antibiotic susceptibility testing can be performed using various methods such as disk diffusion, broth dilution, and automated systems. The results of the susceptibility testing should be interpreted according to the criteria set by the Clinical and Laboratory Standards Institute (CLSI).
Note: The process of blood culture and sepsis diagnosis may vary slightly between different clinical laboratories and healthcare facilities, however, the steps outlined above are the general gold standard procedure.The answers lie within the blood sample.
Yet its quality is inconsistent and often poor.
Our team developed a simple solution to drastically reduce the contamination rate in blood cultures.
Contamination is a common issue with blood culture bottles used for sepsis diagnosis. It occurs when microorganisms that are not related to the patient's infection are introduced into the blood culture bottle, leading to false positive results. This can happen due to various factors, such as improper collection technique, skin or environmental contamination, and poor laboratory practices. Contaminated blood cultures can result in misdiagnosis, inappropriate treatment, and increased healthcare costs.